Macular hole
Description:
The macula is the central area of the retina.Its diameter is around 1mm long. It ensures a subtle and precise vision and most notably it is thanks to the macula that we are able to read.
Any damage caused to the macula impedes visual acuity, distorts perception of images (metamorphopsia) and changes the size and colour of perceived objects.
The macular hole is a loss of retinal substance.
This hole most often appears spontaneously after the age of 60, but can also affect younger patient, notably in the case of high myopia or after a traumatism.
Symptoms:
Without any treatment, the macular hole will gradually expand and cause a potentially major functional disability with the loss of central vision making reading totally impossible.
However the peripheral visual field is preserved and the macular hole does not cause blindness of the affected eye.
Macular hole is caused by posterior vitreous detachment.
The vitreous is a transparent gel which fills the eye and strongly adheres to the retina.
After the age of 60, the vitreous undergoes some changes which lead to its detachment from the surface of the retina. Most of the times, this process goes swiftly but in a few cases, when the adherence of the vitreous to the retina was too strong, the pulling force it creates a macular hole.
Diagnosis:
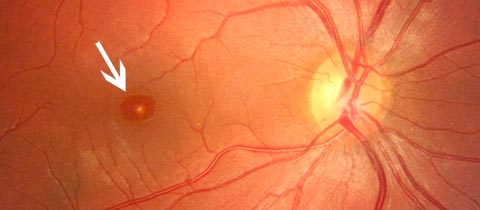
A colour photography (retinography) is useful to compare pre and post-surgery aspects.
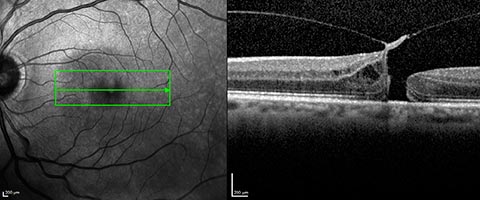
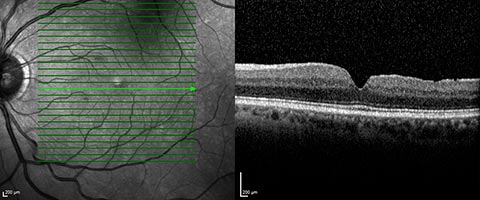
But it is the optical coherence tomography (OCT) which gives the most detailed information (diameter of the hole, thickness of the retina, state of the vitreous…) and allows to best follow the post-surgery evolutions.
Treatment:
The macular hole is treated by surgery. The aim of the intervention is to close the macular hole and therefore reach a functional improvement, but the affected eye will not recover all its former capacities. The visual cells lost during the formation of the hole cannot be recreated.The intervention is usually performed under loco-regional anaesthesia.
The vitreous body is removed (vitrectomy) and a thin membrane is peeled at the surface of the retina (inner limiting membrane).
At the end of the surgery, gas is injected in the eye to help the reattachment of the hole’s sides.
This gas spontaneously resorbs within 15 days, it is gradually replaced by aqueous humor secreted by the eye.
Hospitalization:
The surgery is performed under local anaesthesia and in ambulatory treatment. Patients living alone or far from the surgical clinic might benefit from a short hospital stay.Post-surgery evolution:
Patients don’t usually feel any pain after surgery.A slight sensation of a foreign body within the eye might be felt during the first few days after the operation.
Patients must keep their face facing the ground (the ‘face-down’ position) for 18 to 20 hours a day during 2 to 5 days depending on cases. Maintaining this position is a vital part of recovery
Post-surgery treatment is limited to administering eye-drops.
Travelling by plane or stays in altitude (over 1000m) are forbidden while there is still gas in the eye.
Functional results:
Surgery can achieve the closing of the macular hole in more than 95% of cases.Visual acuity gradually improves over several months and the stage of the final recovery depends on the size and the duration of the macular hole.
In some patients who have not yet been had cataract surgery we might observe an opacification of the eye lens within the few months following the vitrectomy.
Another intervention might therefore be necessary to recover the full benefice of the macular hole surgery.
Complications:
Complications are rare, but can arise as with any other kind of surgery.- The risk of infection: it affects around 2 patients out of 1000. The infection can be efficiently treated by intraocular injections of antibiotics but can sometimes lead to a severe loss of visual functions or even to the loss of the eye.
- Retinal detachment: it affects around 1 patient out of 100, most often within three months after the intervention. It requires another surgical intervention.
- Rise of intraocular pressure or excessive inflammatory reaction requiring a modification of the local (by eye-drops) or general treatment.

 Book an appointment
Book an appointment