Epiretinal and Epimacular membrane
Description:
The macula is the central area of the retina.Its diameter is around 1mm long. It ensures a subtle and precise vision and most notably it is thanks to the macula that we are able to read.
Any damage caused to the macula impedes visual acuity, distorts perception of images (metamorphopsia) and changes the size and colour of perceived objects.
The epiretinal membrane is a thin layer covering the retina in its central area (macula).
This membrane develops spontaneously (in 80% of cases) and touches about 10% of the population over 60.
In 20% of cases, the development of epiretinal membrane comes after a retinal break, a surgery for retinal detachment, an ocular inflammation or retinal vascular disorders.
Symptoms:
The membrane has a slow evolution.It contracts itself and therefore causes the retina to crease, which translates into a decreasing visual acuity and a distortion of perceived objects.
However the peripheral visual field remains untouched and the epiretinal membrane does not blind the affected eye.
Diagnosis:
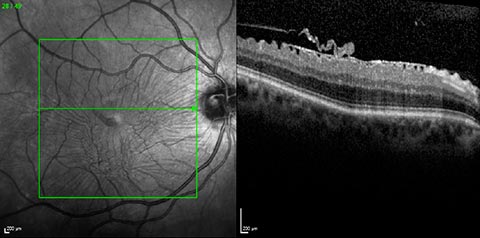
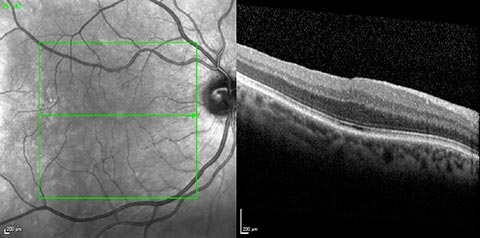
The epiretinal membrane is most often diagnosed with a simple fundus examination. A colour photography (retinography) is often useful to make pre and post-surgery comparisons.An optical coherence tomography (OCT) examination gives more detailed information about the condition (size of the membrane, thickness of the retina, state of the vitreous…) and allows a better follow-up care of post-surgery evolutions.
Treatment:
Surgery is prescribed in the following cases:
- when the visual discomfort increases, so to avoid that it becomes definitive.
- in case of retinal pain.
The surgery consists of removing the vitreous body (vitrectomy) which then allows to remove the membrane with micro surgical forceps.
Hospitalization:
The surgery is usually performed under loco-regional anaesthesia and in ambulatory treatment. Patients living alone or far from the surgical clinic might benefit from a short hospital stay.Post-surgical evolution:
The patient doesn’t usually feel any pain after the surgery.A slight sensation of a foreign body within the eye might be felt during the first few days after the operation.
Post-surgery treatment consists only in the use of eye-drops.
It will be possible for patients to resume all their activities (including driving) within a week.
Functional results:
Visual acuity increases within a few months.Image distortions decrease in 80 or 90% of cases. In 75% of cases patients reach a better visual acuity than before. In other cases vision is at least stabilised and will not decrease any more.
For patients who have not yet benefited from cataract surgery, the eye lens might go through an opacifying process within the next few months after the vitrectomy.
An intervention might therefore be necessary to recover the visual amelioration obtained after the membrane surgery.
Complications:
Complications are rare, but can arise as with any other kind of surgery.- The risk of infection: it affects around 2 patients out of 1000. The infection can be efficiently treated by intraocular injections of antibiotics but can sometimes lead to a severe loss of visual functions or even to the loss of the eye.
- Retinal detachment: it affects around 1 patient out of 100, most often within three months after the intervention. It requires another surgical intervention.
- Rise of intraocular pressure or excessive inflammatory reaction requiring a modification of the local (by eye-drops) or general treatment.
Conclusion:
The results of this type of surgery are good in the vast majority of cases, with a satisfactory functional recovery.In case of an old and persisting epiretinal membrane with a lower natural visual acuity, the recovery prospects are more uncertain.

 Book an appointment
Book an appointment